Depression, anxiety and other mental health problems are incredibly common. It’s estimated that around 1 in 6 people suffer from problems such as these in any given week in the UK(1). Nearly a million people each year are treated by NHS psychological services with an ambition to treat 1.5 million by the year 2020/21. Rates of antidepressant prescriptions are also rising with about 82 people out of every 1000 in the UK now taking antidepressant medication (2).
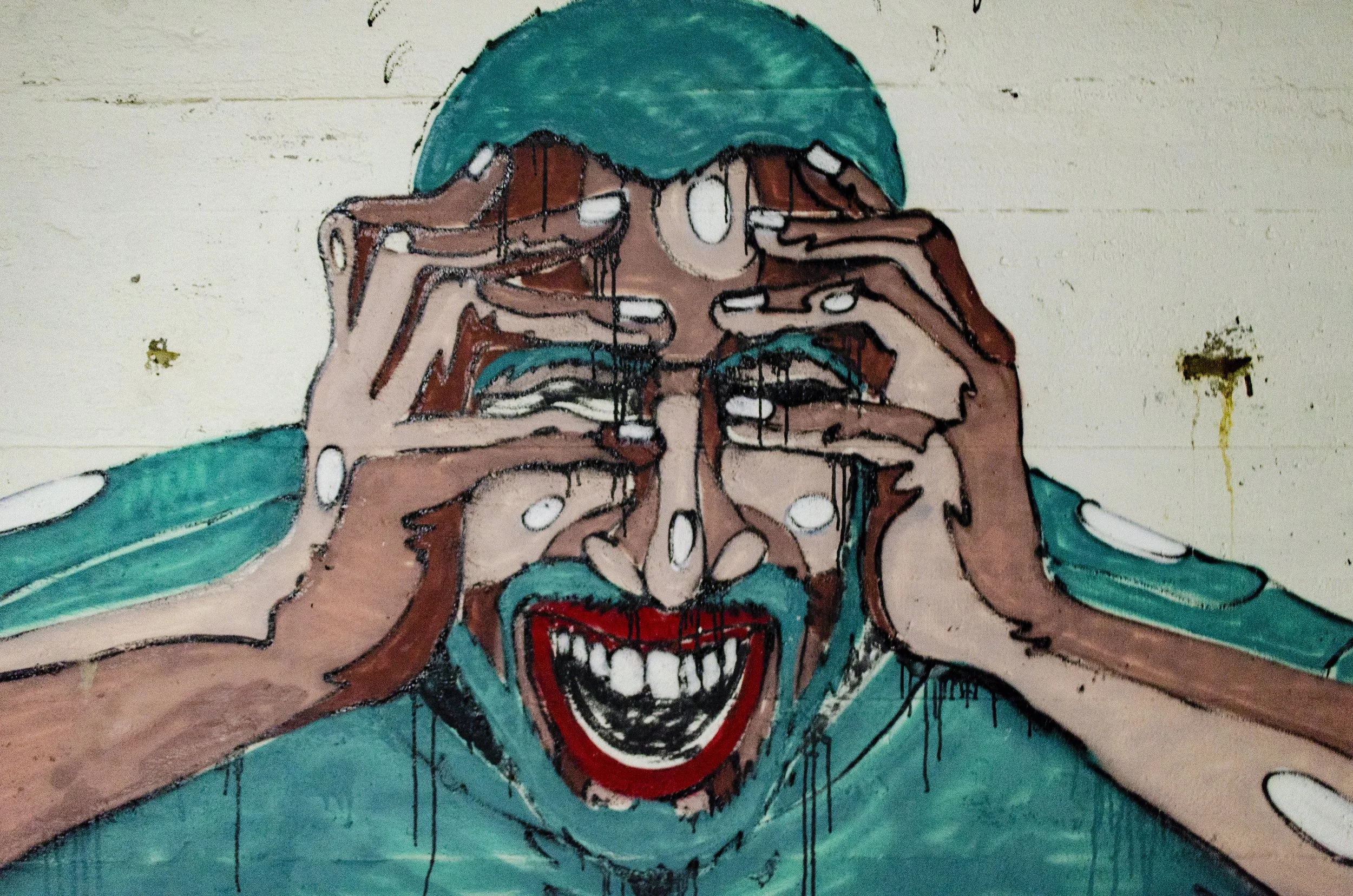
The 2 core features of depression are low mood and loss of interest or pleasure in life, and these usually coincide with other symptoms such as feelings of worthlessness and a sense of fatigue, and when patients come to their GP complaining of a combination of these symptoms they are usually diagnosed with depression.
In the workplace we recognise another mental health condition; the burnout syndrome. Burnout occurs following prolonged periods of unsustainable stress, and occurs most commonly in emotionally demanding occupations with rates of up to 25% in professions such as social work, teaching, and health care (3). In fact some studies amongst doctors have found up to 80% of study participants to be at risk of burnout (4). Whilst it is most common in caring professions, burnout is seen in all working environments from financial services to professional sport.
The three key features of burnout are physical and mental exhaustion, a reduced sense of personal accomplishment in your work, and a sense of ‘depersonalisation’ which is a state of mind where you lose empathy for other people and start to treat them in callous, disinterested ways.
Workload is an important factor in burnout but more important than the amount of work is the inability to choose how that workload is managed which may be because of rigid working practices or micromanagement from above. A feeling of being under-rewarded for the work that you do, either by poor pay or lack of recognition, is also important for burnout. These feelings of not being in control and of not being properly valued are feelings that many people would recognise in their lives outside of work and feelings that contribute in large part to their depression and anxiety.
The similarity between these two conditions – burnout and depression – is striking, particularly the sense of exhaustion which is a very common presenting complaint in depressed patients. They are in fact so similar that I often wonder why we make the distinction, and yet we continue to do so. If a patient comes to me saying they are feeling low and exhausted I am likely to describe them as depressed, but if a colleague tells me they are feeling dissatisfied and exhausted I would describe them as burnt out.
Why does this matter?
The difference is subtle and, just as the symptoms of burnout and depression overlap, so too do many of the treatments so distinguishing between the two may not seem important. But the difference in the labels is important because the attitudinal approach to both feels different. If a person is depressed there is a sense that something is ‘wrong’ with them, it is treated as an illness for which we seek a cure. In contrast if someone is burnt out there is a sense that something is happening to them, they are in a situation that is having a negative impact on them and the focus is usually on trying to improve the situation rather than treating them for an illness.
The NHS is a good example of an environment where burnout is common. Doctors, nurses, and other health professionals are leaving their vocations in droves as a result of it and, albeit slowly, this is raising an awareness that something about the system must change. As a result working practices and even educational curricula at medical schools are changing to try to reduce the rates of burnout. The realisation that the problem of burnout results from the system in which we work is now leading to plans to change the system, rather than just plans to treat individuals when they start to suffer.
Yet amongst the general public there is still more of a focus on treatment than prevention. We are reacting to the groundswell in mental health problems by aiming to put ever more people through psychological therapies and by teaching our children mindfulness techniques at school. This feels like we are teaching people to be able to tolerate a toxic environment, rather than making serious attempts to change the environment that is the source of the problem.
What then if, instead of describing people in society at large as being depressed, we described many of them – arguably more accurately – as being burnt out? This might change our mind set from giving out ever more prescriptions for anti-depressant medication, to one where we look at the systems by which our society operates, and seek to make the changes there.
1. McManus S, Bebbington P, Jenkins R, Brugha T. (eds.) (2016). Mental health and wellbeing in England: Adult psychiatric morbidity survey 2014. Leeds: NHS digital.
2. OECD (2015), Health at a Glance 2015: OECD Indicators, OECD Publishing, Paris,https://doi.org/10.1787/health_glance-2015-en.
3. Mateen FJ, Dorji C; Health-care worker burnout and the mental health imperative. Lancet. 2009 Aug 22;374(9690):595-7
4. Royal College of Anaesthetists. 2017. Morale and Welfare Survey.